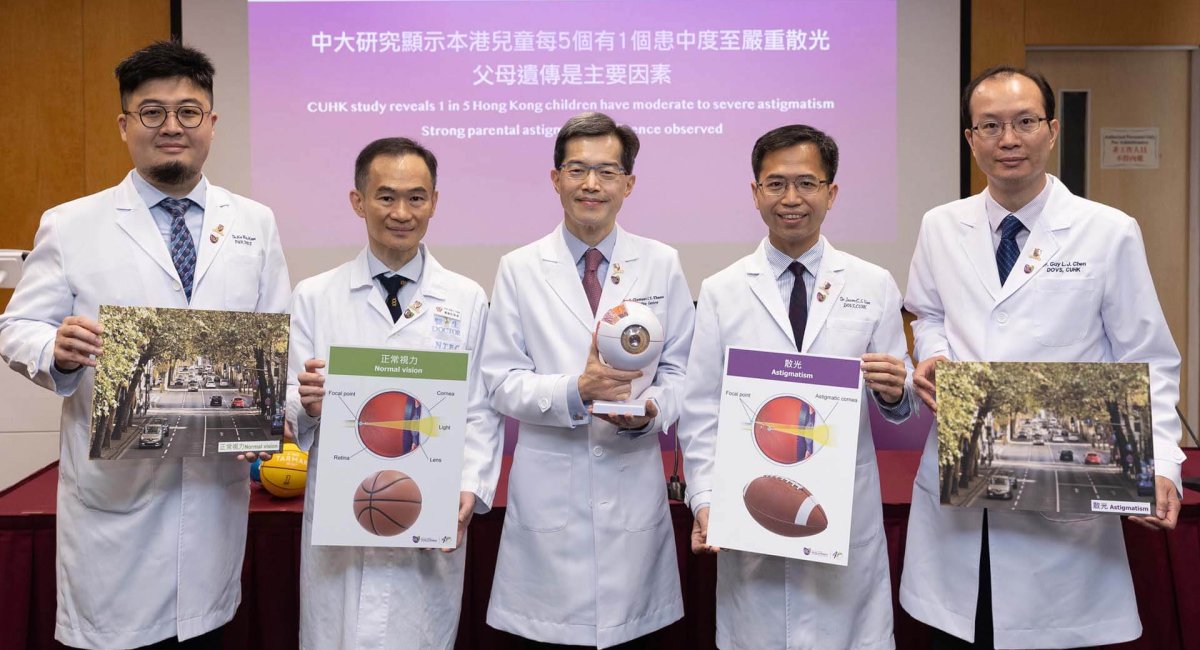
The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) conducted two population-based, cross-sectional studies to evaluate the prevalence of astigmatism in Hong Kong and the association between child and parental astigmatism. Results showed that children in Hong Kong exhibited a higher prevalence of astigmatism than in overseas cities and that 1 in 5 children aged 6 to 8 suffered from moderate to severe astigmatism. Researchers also observed a strong correlation between parental and child astigmatism. Children were at more than three times higher risk of developing astigmatism if both parents had severe astigmatism. Details of the study have been published in the international journals Eye-Nature and JAMA Network Open.
Untreated astigmatism can lead to amblyopia

Astigmatism occurs when the cornea curvatures are unequal, in which circumstance light rays do not converge at a single focal point, leading to the formation of a blurred image.
Prof Clement CY THAM, Chairman and S. H. Ho Professor of Ophthalmology and Visual Sciences of the Department of Ophthalmology and Visual Sciences at CU Medicine, remarked, “Astigmatism prevents a clear vision at any distance during a child’s development which may negatively affect cognitive functions, language ability, and motor tasks. Untreated astigmatism can lead to amblyopia, more commonly known as lazy eye. The golden time of treatment for amblyopia is before the age of eight.”

Prof Guy LJ CHEN, Professor of the Department of Ophthalmology and Visual Sciences at CU Medicine and Associate Director (Medical) of the CUHK Jockey Club Myopia Prevention Programme, added, “Astigmatism has been observed to be more prevalent among Chinese children when compared with other populations. It is usually inherited from the parents. Myopia also plays a role. Studies are now speculating that reading habit is a potential risk factor.”
High prevalence of astigmatism concurs with high prevalence of myopia in HK

CU Medicine’s Department of Ophthalmology and Visual Sciences analysed a total of 3,704 school children and 5,577 adults from the Hong Kong Children Eye Study, which is an ongoing population-based study focusing on eye conditions in primary school children aged 6 to 8 years in Hong Kong. This study aimed to determine the prevalence of astigmatism and evaluate the associations between different astigmatism components, including refractive astigmatism (RA) and corneal astigmatism (CA).
Results showed school children in Hong Kong has a greater RA (21.9%) and CA (63.9%) prevalence than in other parts of the world. An association of astigmatism with myopia was confirmed as well (see details in Table 1).
Table 1: Prevalence of astigmatism in children and adults in Hong Kong
| Children | Adults | |
| Refractive astigmatism ≥ 0.5 D | 63.6% | 70.0% |
| Corneal astigmatism ≥ 0.5 D | 95.8% | 75.6% |
| Refractive astigmatism ≥ 1.0 D | 21.9% | 30.9% |
| Corneal astigmatism ≥ 1.0 D | 63.9% | 39.5% |
Dr Jason CS Yam, Associate Professor of the Department of Ophthalmology and Visual Sciences at CU Medicine and Director of the CUHK Jockey Club Myopia Prevention Programme, said, “Astigmatism is known for its association with myopia. Hong Kong is among cities with the highest prevalence of myopia in the world, affecting more than 40% of school children at the age of eight. This may explain why we also have a high prevalence of astigmatism. The high prevalence of astigmatism among both children and adults has led us to ask the next question. How is parental astigmatism going to affect their child?”
Child CA risk is three times higher if parents have high astigmatism
To answer that question, the research team looked at 5,708 family trios, consisting of a child and both parents, in order to investigate the influence of parental astigmatism on children. Examining data from 17,124 subjects, researchers concluded that among other reported biological, environmental, and sociodemographic factors, parental astigmatism was shown to be the most important factor associated with child astigmatism and both parents were associated with the inheritance of astigmatism. The team categorised children into six groups based on the severity of astigmatism of both parents and calculated the corresponding risks in their children (see details in Table 2).
Table 2: The association of parental astigmatism on child astigmatism in 5,708 trios
Child RA risk
| Both parents having moderate astigmatism | Child RA risk is 60% higher than children whose parents had no astigmatism |
| Both parents having severe astigmatism | Child RA risk is 2 times higher than children whose parents had no astigmatism |
Child CA risk
| Both parents having moderate astigmatism | Child CA risk doubled that of children whose parents had no astigmatism |
| Both parents having severe astigmatism | Child CA risk is 3 times higher than children whose parents had no astigmatism |

Dr KAM Ka-wai, Clinical Assistant Professor (honorary) of the Department of Ophthalmology and Visual Sciences at CU Medicine and Associate Director (Education) of the CUHK Jockey Club Myopia Prevention Programme, said, “To the best of our knowledge, this is the first population-based, cross-sectional study to quantify the associations of parental astigmatism with child astigmatism. We found that the prevalence of both RA and CA in children increased with both the number of parents with astigmatism and the severity of parental astigmatism. For example, children were at 62% higher risk of RA if both parents had moderate astigmatism (of 1.0 dioptre of more). And, the risk of child CA nearly doubled if both parents had moderate astigmatism of ≥1.0D and increased by more than three times if both parents had severe astigmatism of ≥2.0D.”

Prof Alvin L YOUNG, Clinical Professor (honorary) of the Department of Ophthalmology and Visual Sciences at CU Medicine, remarked, “The stratification into six groups serves as a clinical guide for clinicians when they counsel parents with astigmatism, in addition to allowing better triage of resources and targeting of preschool children of astigmatic parents for any uncorrected astigmatism. Children with parents with astigmatism should have an early eye examination for a timely detection of astigmatism so that appropriate vision correction can be initiated for a healthy visual development.”


2023年5月30日
中大研究顯示本港兒童每5個有1個患中度至嚴重散光 父母遺傳是主要因素
散光是世界上最常見的屈光不正現象,比近視或遠視還要普及。倘若散光患者在視力發育階段沒有得到治療,嚴重的散光可導致弱視。香港中文大學(中大)醫學院早前進行了兩項研究,評估本港的散光患病率,並分析兒童與父母患散光的關聯。結果顯示,本港兒童患上散光的比率較其他海外城市高,而每5個年齡介乎6至8歲的學童當中便有1個患上中度至嚴重散光。研究團隊亦證實父母的散光度數與子女患散光的風險及程度有密切關聯。若父母兩人同時患有嚴重散光,子女患上散光的風險會增加3倍以上。研究詳情已在國際醫學期刊《Eye-Nature》及《JAMA Network Open》上發表。
嚴重散光可導致弱視
散光主要成因是眼角膜弧度不規則,由於光線經角膜進入眼球未能匯聚在單一的焦點,導致眼睛所見的影像模糊。
中大醫學院眼科及視覺科學學系系主任兼何善衡眼科及視覺科學講座教授譚智勇教授解釋:「患有散光的人不論看近或遠的景物都會模糊不清。散光可間接影響兒童的認知、語言及運動發展,若未經治療可導致弱視,俗稱「懶惰眼」。一旦錯過八歲前的黃金治療時期,視力便有機會永久受損。」
中大醫學院眼科及視覺科學學系教授兼「香港中文大學賽馬會瞳心童行計劃」副總監(醫療)陳理佳教授補充:「文獻指出華人兒童患散光的比率較其他種族高。主要原因是遺傳,其他因素包括深近視,亦有研究指出閱讀習慣或許會增加散光。」
香港患散光比率高與高近視人口一致
中大醫學院眼科及視覺科學學系研究團隊從其「香港兒童眼科計劃」中收集3,704名學童及5,577位成年人的數據進行散光研究分析。「香港兒童眼科計劃」是學系由2015年開始的研究計劃,經全港小學轉介6至8歲學童,為他們提供免費的全面眼科檢查,從而了解本港學童的眼睛健康狀況。是次研究主要探討本港學童及成人患散光的比率,並分析不同散光種類以及其關聯,當中包括屈光散光和角膜散光。結果顯示,本港學童患屈光散光及角膜散光的比率較其他城市高,分別為21.9%及63.9%。團隊亦證實近視度數會影響散光度數的增減(詳細數據見附表一)。
表一: 本港兒童及成人的散光患病率
| 兒童 | 成人 | |
| 患50度或以上屈光散光 | 63.6% | 70.0% |
| 患50度或以上角膜散光 | 95.8% | 75.6% |
| 患100度或以上屈光散光 | 21.9% | 30.9% |
| 患100度或以上角膜散光 | 63.9% | 39.5% |
中大醫學院眼科及視覺科學學系副教授兼「香港中文大學賽馬會瞳心童行計劃」總監任卓昇醫生表示:「近視度數的增減與散光息息相關。香港作為全球近視患病率最高的城市之一,有四成以上的8歲學童患有近視,這或可解釋為何我們的散光患病率同樣高企。我們今次的研究揭示了散光在香港的成年人及兒童當中都是相當普遍的,正因為我們的散光患病率亦比鄰近地區高,所以我們想進一步了解父母患散光有否影響他們的小朋友。」
父母有嚴重散光 子女患角膜散光的風險高三倍
團隊於是邀請了5,708名學童以及其父母,共11,416名家長,調查父母患散光對子女患散光的直接影響。他們分析數據後得出結論,證實在生理、環境和社會人口等因素當中,父母遺傳是兒童患散光的最重要風險因素。團隊繼而根據父母雙方的散光嚴重程度將兒童分為六組,並計算出相關患病風險(詳見附表二)。
表二: 研究的5,708個家庭組合中父母與子女患散光的關聯
兒童屈光散光
| 父母雙方均患有中度散光 | 兒童患屈光散光的風險較父母沒有散光的兒童高60% |
| 父母雙方均患有嚴重散光 | 兒童患屈光散光的風險較父母沒有散光的兒童高2倍 |
兒童角膜散光
| 父母雙方均患有中度散光 | 兒童患角膜散光的風險較父母沒有散光的兒童高1倍 |
| 父母雙方均患有嚴重散光 | 兒童患角膜散光的風險較父母沒有散光的兒童高3倍 |
中大醫學院眼科及視覺科學學系名譽臨床助理教授兼「香港中文大學賽馬會瞳心童行計劃」副總監(教育)甘嘉維醫生表示:「據我們所知,這是第一個覆蓋整體人口及針對散光進行的橫向研究,以量化父母患散光與其子女患散光的關聯。我們發現兒童的屈光散光和角膜散光患病風險會隨父母雙方的患散光人數及程度增長。例如,父母各有100度屈光散光,小朋友患上屈光散光的風險會增加62%。另一例子,父母雙方患有100度或以上散光,小朋友患角膜散光的風險會增加94%。倘若父母雙方患有200度或以上散光,小朋友的患角膜散光風險會增加3倍以上。」
中大醫學院眼科及視覺科學學系名譽臨床教授楊樂旼教授總結:「我們歸納出的六個組合,為父母及醫護人員提供一個臨床參考,可以更精準地分流醫療資源,以篩查帶有高散光風險而未曾獲得診斷的學齡兒童。我們鼓勵患有散光的父母應盡早為子女安排眼科檢查,及時發現散光,透過合適的鏡片矯正視力,以確保眼睛健康發育。」
 Creative Commons Attribution
Creative Commons Attribution