In the Asia Pacific region, the condition of central serous chorioretinopathy (CSCR) is reportedly more prevalent than in other populations. If left untreated, chronic CSCR, lasting more than three months, can lead to permanent sight loss. Our team is dedicated to improving the diagnosis, evaluation, classification, and treatment of CSCR through our research projects. We conducted a retrospective review to investigate the long-term efficacy and prognostic factors of photodynamic therapy (PDT) in chronic CSCR. The results showed that half dose PDT achieves long-term stable visual acuity and rapid resolution of serous retinal detachment. The main outcome of our study was the recommendation that patients undergo PDT treatment before vision deteriorates to achieve best visual acuity outcomes. In addition, those patients with more complex CSCR (multifocal CSCR) should be more closely monitored for recurrence.
One of the limitations of PDT therapy is the cost, and in Hong Kong this is a self-funded item. Therefore, another novel laser therapy, subthreshold micropulse yellow (577nm) laser (SML), was tested by our research team and found to be effective in treating chronic CSCR. Micropulse laser is free for patients in the Hospital Authority. Our large scale randomized controlled clinical trial comparing SML and half-dose PDT for CSCR showed SML to be noninferior to half dose PDT in the treatment of CSCR both in terms of resolving subretinal fluid and improving vision.
Our genetic research team have identified associations of ARMS2, CFH, and TNFRSF10A with CSCR and revealed that these genes may affect different phenotypic expressions of CSCR, neovascular age-related macular degeneration (nAMD), and polypoidal choroidal vasculopathy (PCV).
In addition to investigating the effectiveness of therapies, we also work to study the diagnosis and classification of CSCR through retinal and choroidal imaging. In the past, it was difficult to frequent monitor the status of abnormal choroidal vessels in CSCR patients since fluorescence angiography is invasive method that involves infusion of dye. The sweep-source optical coherence tomography angiography (OCTA) made it possible to obtain quick structural images of the choroid to analyze and study the relationship of choriocapillaris perfusion in CSCR patients. We have reported on the changes in choriocapillaris appearance following PDT and SML treatment.
Dr Mårten BRELÉN also developed the first preamplified electroretinography (ERG) recording electrode and validated its usefulness in a range of ERG recordings. This novel ERG electrode is now being tested in a variety of different retinal and macular diseases, including CSCR. In the past few years, we have published in journals, including Journal of Ophthalmology, American Journal of Ophthalmology, British Journal of Ophthalmology and Translational Vision Science & Technology. Dr. Brelen also obtained patents from China National Intellectual Property Administration for ‵active electrode detection device for electroretinogram and electro-oculogram′ (CN 107582053 B).
Glaucoma is the most important cause of irreversible blindness in Hong Kong. Primary angle closure glaucoma (PACG) is a subtype of glaucoma with higher morbidity and risk of blindness, and has the highest prevalence in Chinese. We conduct intensive research programs on PACG. Our group is widely regarded as one of the leading clinical research groups on the surgical management of PACG in the world.
Since 2005 we have conducted three landmark randomized controlled clinical trials that established the efficacy and safety of lens extraction (of cataractous or even ‵clear′ lenses) as one of the viable first-line surgical options in the management of iridotomized PACG eyes. Lens extraction reverses, at least partially, the anatomical predisposition to angle closure in PACG eyes, reduces intraocular pressure (IOP) and the requirement for glaucoma drugs, and facilitates subsequent glaucoma lasers or surgeries, in particular those that involve the drainage angle.
In our earlier randomized controlled trial on acute primary angle closure (APAC), we established argon laser peripheral iridoplasty (ALPI) as an effective and safe first-line intervention for APAC. Another randomized controlled trial by our research group confirmed that early lens extraction was more effective than conventional laser peripheral iridotomy in preventing the progression to chronic PACG after an acute angle closure attack. Our 10 years′ follow-up results suggested that patients who underwent early lens extraction required less glaucoma medications to control the intraocular pressure and had lower incidence of blindness. The paper was selected as ‶paper of the month″ by the Associate Advisory Board of the World Glaucoma Association in April 2021.
Our other research interests in PACG also include (1) The clinical efficacy and safety of other surgical interventions in PACG eyes, including laser peripheral iridotomy and iridoplasty, trabeculectomy (penetrating, non-penetrating, carbon dioxide laser-assisted), goniosynechialysis (GSL), glaucoma implant surgery, laser cyclodestructive procedures (transscleral and endoscopic), and various combinations of the above; (2) The anatomical effects of surgery on the anterior segment structures in PACG eyes; (3) Diurnal intraocular pressure profiles in PACG eyes, and the impact of different treatments on pressure fluctuations; (4) cost-effectiveness of treating PACG with different surgical techniques, and (5) the genetic basis of PACG.
Our glaucoma research group has published 4 original papers in Nature Genetics in collaboration with international consortium (Journal impact factor: 27.605 in 2019; Journal Rank: 2/178 in Genetics & Heredity in 2019), 13 original papers in Ophthalmology (Journal impact factor: 8.470 in 2019; Journal Rank: 3/60 in Ophthalmology in 2019), and a total of 43 original papers. Our Principal Investigator, Prof. Clement C.Y. Tham, an internationally-recognized authority on PACG, has been invited to present 9 Named / Award Lectures and over 190 invited symposium lectures and instruction courses on the management of PACG in international scientific congresses, including the prestigious Honored International Lecture at the annual scientific meeting of the American Society of Cataract and Refractive Surgeons (ASCRS), the APAO De Ocampo Lecture, and the APAO Holmes Lecture.
Myopia (short-sightedness) is the most common ocular disorder worldwide and a global health threat to most populations. It is associated with excessive eyeball growth that leads to sight-threatening complications. Hong Kong has one of the highest prevalence of myopia in the world: 12% of 6-year-olds, 24% of 7-year-olds, 33% of 8-year-olds and 95% of university students. We conduct intensive research programs on myopia. Our group is widely regarded as one of the leading myopia research groups worldwide.
We have conducted the world′s first randomized placebo-controlled clinical trial on low-concentration atropine eye drops for myopia control, the Low-concentration of Atropine for Myopia Progression (LAMP) study. We determined 0.05% atropine as the optimal concentration which can reduce the myopia progression rate by 67%. Its anti-myopia effect is mainly via slowing down axial elongation and therefore can reduce future myopia complications. Young children tend to progress fast, and require a relative higher concentration for adequate myopia control. Our findings establish the treatment protocol for this emerging and promising therapy, which confer clinical impact to millions of children suffering from fast progressing myopia.
We have also conducted a population-based study Hong Kong Children Eye Study, an epidemiological cohort of 30,000 children and their parents for detailed phenotypic and genotypic characterization. We have identified conventional risk factors of near work and limited outdoor activities, as well as newly found effects of life style and parental influence on myopia progression. We found that parental myopia confers the strongest and dose-dependent risk on childhood myopia development. Recently, we draw world media′s attention by identifying adverse effect on children′s eye features by passive smoking and genetic factors for myopia. We are the leading group to advance the early detection of amblyopia based on choroidal vasculature. We advocate the new concept of children health care through eye care.
We also establish the Hong Kong High Myopia Cohort, which include evaluations of: (1) Myopia-related fundus changes and visual prognosis in Hong Kong children and adults with high myopia. (2) Global assessment of choroid and scleral changes in high myopia of Hong Kong children and adults. (3) Functional visual ability and quality of life in children with high myopia. (4) Genetic basis of high myopia.
Our myopia works are supported by more than 7 million USD research grants. Our results have been published in more than 20 original articles with the Department as the corresponding institution between 2016 and 2020, including publications in Ophthalmology, JAMA Ophthalmology, American Journal of Ophthalmology, British Journal of Ophthalmology, and Acta Ophthalmologica. Our Principal Investigator, Prof. Jason Yam, an internationally-recognized authority on myopia, has been invited to present 7 Award / Keynote Lectures and over 70 invited symposium lectures on myopia in international scientific congresses. Our work has been recognized by multiple awards including Asia Pacific Academy of Ophthalmology (APAO) Nakajima Award, APAO Distinguished Service Award, APAO Outstanding Service in Prevention of Blindness, Asia-Pacific Strabismus and Paediatric Ophthalmology Society Young Investigator Award, Gold Medal for Best Original Research by Young Fellows in Hong Kong Academy of Medicine.


Retinoblastoma (RB) is the most common malignant intraocular cancer accounting for about 4% of cases of all pediatric cancer. The incidence of RB is recorded to be about 5 – 10 new cases annually in Hong Kong. About 40% of RB are hereditary and the rest are sporadic. Patients with hereditary RB are predisposed to non-ocular cancer later in life with 30% to develop secondary tumors after 40 years and 22% to develop tertiary tumors. The most common presenting signs and symptoms are leukocoria and strabismus. Prognosis is highly dependent on the time of diagnosis. Late presentation with extraocular spread is often fatal; while curable using systemic and focal therapy in the early stage. However, RB is often diagnosed in relatively later stages, as early detection requires vigilant screening and public awareness. Our group conduct intensive research and programs on Retinoblastoma, and actively participate in the international working group.
RB1 gene responsible for regulating cell growth is associated with the tumorigenesis in RB. We have conducted extensive studies on the RB1 gene and other RB-related genes for the better understanding of the disease mechanism. We have found that about 19% of RB patients in Hong Kong Chinese carry a germ-line RB1 mutation with no methylation at the RB1 promoter. For most of the patients, we found that the RB1 gene is inactivated by loss-of-function mutations and loss of heterozygosity. We identified epigenetic silencing of DNA repairing genes (MGMT 35% and MLH1 67%) and tumor suppressor gene (RASSF1A 82%) in RB, loss of heterozygosity at chromosomal regions of D19S902 and D22S539. We have also found upregulation of B lymphoma Mo-MLV insertion region 1 (BMI-1) protein related to the invasion of the cancer cells.
We have also successfully induced cell death of RB by a novel method. Our previous study found that GHRH, GHRH-R and GH are highly expressed in the retina. We have successfully induced cell death of RB by GHRH-R antagonists. We also found that deficiency in the RB protein would allow cells to employ a more error-prone pathway to repair broken DNA, which would compromise the overall genome stability and lead to higher tendency of tumorigenesis. Clinically, chemoreduction has been used for the RB management which jeopardize conjunctival wound healing, we have also reported the use of topical autologous serum in promoting healing of conjunctival wounds.
Apart from conducting intensive research on RB, we have also launched city-wide Hong Kong Retinoblastoma Awareness and Education Campaign with Children′s Cancer Foundation and Department of Health in 2017 to raise the public awareness of RB for early disease detection and improved outcomes. We have also established Hong Kong Retinoblastoma Registry in 2020 to document cancer incidence, mortality rates in Hong Kong and detailed information such as clinical presentations, staging, treatment modalities and long-term outcomes which would provide more accurate and comprehensive data and allow in-depth study of the epidemiology and characteristics of RB.
We have published 14 original articles in Retinoblastoma with the Department as the corresponding institution between 2002 and 2021. We have published in major journals, including Lancet Global Health, JAMA Oncology, Proceedings of the National Academy of Sciences of the United States of America, Ophthalmology, and Investigative Ophthalmology and Visual Science, and three book chapters in Advances in Vision Research Volume I, II and III. Our work has been bestowed the Kowloon Central Cluster Outstanding Team Award of Hospital Authority in 2020. Our principal investigator, Prof. Jason Yam, an internationally recognized authority on Retinoblastoma, has joined the Global Retinoblastoma Study Group, One Retinoblastoma World Network and Global Retinoblastoma Presentation 2017 Study.

Thyroid Eye Disease (TED) is a severe extrathyroidal manifestation of autoimmune thyroid diseases, and the most common orbital disorder in adults worldwide. TED is an eye disease that leads to 4Ds: Dysfunction, Double vision, Discomfort and Deformities (Below, Right).
Accordingly the Thyroid Eye Clinic at New Territories East Cluster (TEC@NTEC) was set up as the first dedicated medical service in Hong Kong for TED. Since the fall of 2010, the team has managed over 1200 new TED patients. Spearheaded by Dr Kelvin Chong, TEC@NTEC has seamless connection with the Chinese University of Hong Kong Eye Centre (CUHKEC), Eye Centre at CUHK Medical Centre (CUHKMC), the research laboratory at the Department of Ophthalmology and Visual Science, as well as a multidisciplinary team of endocrinologists, paediatricians, radiation oncologists, endocrine surgeons and radiologists. TEC@NTEC facilitates therapeutic, technical and translational development in TED, and was recently recognized as the ‶NTEC Outstanding Team″ in 2020 (left)

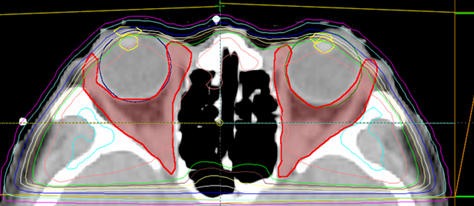
Our collaborative work with the Department of Imaging and Interventional Radiology (DIIR) establishing 3T multiparametric Magnetic Resonance Imaging (mpMRI) protocol for image-guided treatment in progressive TED is an important breakthrough enhancing the standard of care of TED patients in the Asia Pacific region (S. K. Yee Medical Foundation 2020). European consensus and recommendation relies exclusively on clinical (bedside) examination for assessment and treatment options. Our local experience confirm substantial ethnic-related differences on the presentations and progression of Chinese TED patients. Adopting 3T-MRI provide sensitive and objective detection of ‶clinically subtle″ TED activity and severity and directs the individualized use of medical (progressive, early disease) or surgical treatments (fibrotic, stable disease).

Our collaborative work using 3T-MRI to evaluate the inflammation and expansion of extraocular muscles before and after immunosuppressive treatments was recently awarded the ‶Best Presentation at the European Group on Graves Orbitopathy (EUGOGO) 20th Anniversary Meeting″. We further expand the use of 3T-MRI to assess the common and symptomatic involvement of lacrimal glands in our cohort. This correlates with eyelid swelling and dry eye severity and supporting the use of periocular steroid injection for Thyroid-Associated Symptomatic Dry Eye (TASDE).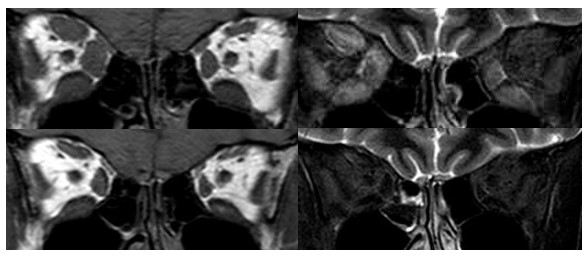
3TMRI images showing severe (T1Weighted, left), radiologically active (STIR, right) TED
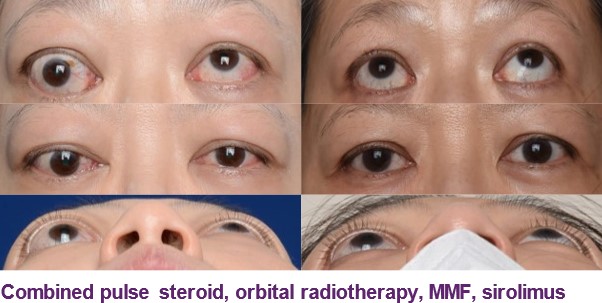
Before (above) and after (below) combined triple immunosuppression
Combining clinical, radiological and immunological evaluation, our team has developed a staged immunosuppressive protocol using pulse steroid, orbital radiotherapy and/or oral immunosuppressant as definitive or neoadjuvant treatment for dysthyroid optic neuropathy (DON) or extraocular myopathy (intractable/progressive diplopia) or orbitopathy. We have accumulated first-hand experience of different immunosuppressants from methotrexate, azathioprine, mycophenolate, sirolimus to biologics including Rituximab and Tocilizumab in treatment-refractory TED.
DON is an uncommon yet sight-threatening complication of TED. We have been promoting the use of combined medical and surgical decompression for over 10 years as a personalized management with improved safety (risk of diplopia) and efficacy (relief of DON). We are among the world′s first groups of ophthalmologists to independently conduct ‶Endoscopic Transethmoidal Medial Orbital Wall Decompression for Dysthyroid Optic Neuropathy″ which was awarded the ‶Best of Video Show award″ by the American Academy of Ophthalmology in 2011. We also introduced navigation guided orbital decompression for training and demonstration. (SK Yee medical foundation 2019).
Endoscopic Navigation during orbital apical decompression for dysthyroid optic neuropathy
To avoid unpleasant skin scarring, common in Asian patients after rehabilitative orbital decompression for proptosis reduction, we also develop ‶Scar-less Approach for Deep Lateral Wall Orbital Decompression″ which was awarded the ‶Top Surgical Video Award″ during the World Ophthalmology Congress in 2018.

Our multidisciplinary translational research focuses on the development of
(1) serologic biomarkers including thyroid-stimulating hormone receptor (TSHR) and insulin-growth factor-1 receptor (IGF-1R) based tests to identify patients at risk of progressive TED
(2) photographic biomarkers using explainable AI-based deep learning technology (Faculty of Engineering and Medicine – Research Sustainability of Major RGC Funding Schemes 2019)
(3) imaging biomarkers including Optical Coherence Tomography (OCT) and OCT angiography in patients with congestive orbitopathy or compressive optic neuropathy (below, left)
(4) radiological biomarkers in 3T-MRI and AI-based deep learning for progressive TED (GRF 2020)
(5) genetic biomarkers in TED using next generation sequencing (GRF 2020)
(6) TED animal models for therapeutic targets with UK and German groups
Orbital fat and eye muscle expansion and infiltration are key pathological changes in TED. We have for the first time, established a site-specific (orbital versus subcutaneous fat) stem-cell model through which we identified the specific roles of bone morphogenic proteins in TED.
As one of the three founding board of directors from Asia in International Thyroid Eye Disease Society (ITEDS), Dr Chong actively participates in educational activities (Education Director, ITEDS) and multi-center clinical studies led by ITEDS. He served as the past President of the Hong Kong Society of Ophthalmic Plastic and Reconstructive Surgeons (HKSOPRS) and the past first Vice President of Asia Pacific Society of Ophthalmic Plastic and Reconstructive Surgeons (APSOPRS), the two professional bodies for oculoplastic surgeons in Hong Kong and Asia Pacific regions who specialize in the management of TED. We recently organized an APSOPRS-ITEDS webinar on ‶TED – East meets West : therapeutic, technical and translational updates″ in 2021.

CUHK DOVS conducts research in genomics and molecular biology of complex eye diseases, including age–related macular degeneration (AMD), polypoidal choroidal vasculopathy (PCV), central serous chorioretinopathy (CSCR), diabetic retinopathy and maculopathy, primary open–angle glaucoma (POAG), primary angle–closure glaucoma (PACG), keratoconus, and myopia. These diseases are common and can be blinding. We also study inherited retinal dystrophy (IRD), congenital glaucoma, corneal dystrophy, and retinoblastoma, which are rare monogenic diseases with severe consequences. We also initiated research on the genetics of ocular traits in children, including refractive errors (including myopia and myopia progression), axial length, intraocular pressure, corneal thickness, retinal nerve fiber layer, and retinal vasculatures.
In AMD and PCV, we have made important discoveries in identifying the PGF, ANGPT2, TIE2, and ABCG1 genes as new susceptibility genes for neovascular AMD and PCV. In HTRA1, a susceptibility gene to exudative AMD that we discovered in 2006, we have revealed a variant had higher cell viability, lower cell apoptosis and was less responsive to anoikis, indicating a rare protective role. We identified a protective AMD-associated HTRA1 variant, c.34delCinsTCCT in AMD pathogenesis due to its role in RPE cell degeneration. Through delineation of the genetic profiles of neovascular AMD and PCV, we found association of AMD-associated genes with PCV, but HTRA1 variants had significantly stronger effects on neovascular AMD than on PCV. We have thus discovered overlapping genetic components of neovascular AMD and PCV. In comparative genetic analysis of neovascular AMD, PCV and CSCR, we have found that the major risk alleles in the CFH and ARMS2/HTRA1 genes are protective for CSCR, suggesting allelic diversities among the three common maculopathies. Our team plays a leading role in the genetic differentiation among neovascular AMD, PCV and CSCR.
In glaucoma, we have identified specific genetic association patterns of multiple genetic loci with POAG and PACG, including the CAV1–CAV2, SIX1–SIX6, FOXC1 and PARL–ABCC5–HTR3D–HTR3C, contributing to establishing the complex genetic architecture of glaucoma.
In myopia, apart from identifying new genes and variants, we also pioneered investigation of the genetic components in different severities of myopia: mild, moderate and high myopia. We identified variants in the PAX6, ZC3H11B, ZFHX1B and SNTB1 genes that confer stronger effects on higher-grade myopia. These genes therefore have become candidates for genetic screening and prediction for patients with high myopia.
In peripheral sclerocornea, a corneal opacity disease, we have identified a heterozygous mutation of RAD21 which leads to disorganization of collagen fibres in the cornea stroma. Mechanistically, this mutation affects the 3D chromosome organization and the expression of cell adhesion gene cluster PCDHG, which reduces neural crest migration and corneal stroma development during embryo development. This is a new understanding in the pathogenesis of corneal diseases.
In retinoblastoma, we have determined its novel association of the GHRH-GH-IGF1 axis. We revealed the involvement of GHRH-R in survival and proliferation of retinoblastoma and showed that GHRH-R antagonists can specifically kill the RB cells.
In children eye traits, we have investigated the genetic components of refractive errors, axial length, intraocular pressure, central corneal thickness, and retinal nerve fiber layer (RNFL) thickness. We are the first group to prove the association of ZC3H11B and BICC1 with moderate and high myopia, and ZC3H11B, KCNQ5, SNTB1, GJD2, WNT7B and RSPO1 with excessive axial length in children. Also, we have for the first time identified variants in the ZFHX1B, KCNQ5 and GJD2 genes to be associated with myopia progression in children. Also, we have found SIX6 variants to be associated with peripapillary RNFL thickness in children, with age- and sex-specific effects.
We have published 35 original articles in eye genetics with the Department as the corresponding institution between 2016 and 2021. We also collaborated with international consortium on eye research and identified a number new genes and variants for wet AMD, PCV, glaucoma, and myopia, which leads to another 21 publications. We have published in major journals, including Lancet Oncology, Nature Genetics, Nature Communications, American Journal of Human Genetics, Proc Natl Acad Sci USA, Genetics in Medicine, Human Molecular Genetics, Ophthalmology, British Journal of Ophthalmology, and Investigative Ophthalmology & Visual Science.
CUHK DOVS conducts research in ocular imaging, focusing on development and application of image analysis techniques and artificial intelligence (AI) for studying common eye diseases (e.g. glaucoma and diabetic retinal disease). We have published more than 100 publications in international peer-reviewed journals and book chapters related to ocular imaging, with several landmark papers on development of quantitative analysis for optical coherence tomography angiography, and AI-based technologies for analyzing ocular images. We have secured external funding from General Research Fund (GRF) and Research Matching Grant from the Research Grants Council (RGC), the Health and Medical Research Fund (HMRF), the Innovation and Technology Fund (ITF) from Innovation and Technology Commission (ITC), and the BrightFocus Foundation. The findings from these research studies have impacted on understanding of eye diseases leading to a more targeted and effective screening strategy and risk assessment for prevention of blindness using state-of-the-art ocular imaging technology, which has immense potential to lead to impactful benefits to both science and society.
Currently, we are now focused on translating our ocular imaging related research from ‶concept″ to ‶real-world clinic″. For example, the research team led by Dr Carol Cheung is conducting a pilot study to deploy our AI algorithms into Hospital Authority (HA) hospitals to enhance eye disease screening, triaging and referral pathway for timely eye disease treatment and management. Implementation of our AI algorithms will largely improve the efficiency of current clinical workflow, reduce the workload for the ophthalmologists, and decrease the waiting time for eye examinations meanwhile maintaining a low screening cost in the public service in Hong Kong. We are also pioneering to use AI-based retinal imaging to screen Alzheimer′s disease for aiding early disease detection. Our AI work will bring significant societal impact by improving quality and efficiency of healthcare system, and enhancing patient outcomes. Moreover, it will be set as a model for translating AI research in medicine.
In addition, the research team collaborates with different researchers all around the world, and the international collaborative work has been published in high-impact journals including the New England Journal of Medicine (NEJM), JAMA, The Lancet Digital Health, Nature Biomedical Engineering and Diabetes Care.